What to Expect, Dos & Don'ts of Transmyocardial Revascularization (TMLR)
Despite improvements in the medical and surgical treatment of coronary artery disease (CAD), many individuals continue to experience symptoms even after trying all of the standard treatments. These individuals typically continue to experience chest discomfort after receiving the most effective medical treatment, and the majority are extremely vulnerable to surgical intervention.
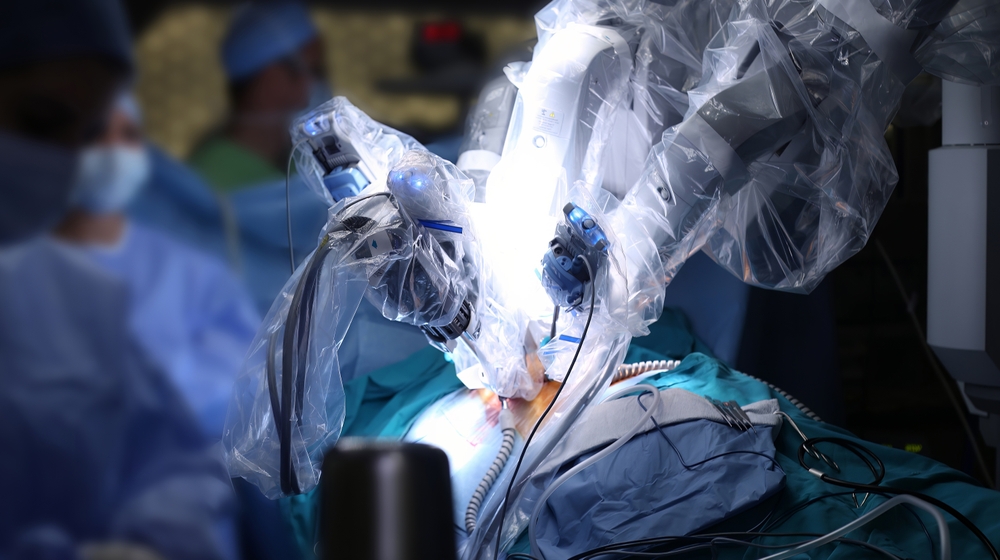
A powerful carbon dioxide laser or other laser is used in transmyocardial laser revascularization (TMLR), which involves vaporizing the ventricular muscle and generating a 1-mm-wide transmural conduit in the left ventricle. Its exact physiologic mechanism of action is not well understood.
Many patients benefit from coronary artery bypass grafting (CABG), although some are not suited for direct revascularization operations. The growing interest in TMLR for the treatment of CAD that would otherwise be surgically incurable has generated much interest. Numerous sizable clinical investigations have revealed significant advancements in angina. After TMLR, these benefits begin immediately and continue. Regional myocardial perfusion may also be enhanced, however, thallium scintigraphy has not been able to conclusively demonstrate this.
Types of TMLR:
- Transmyocardial laser revascularization (TMLR): To do transmyocardial laser revascularization, a small incision must be made on the left side of the chest. A laser is then used to drill minuscule channels into the heart muscle. There is no need for a heart-lung bypass machine since the heart beats continuously throughout the treatment.
- Percutaneous transmyocardial revascularization (PTMR): Through a small skin incision, a catheter-guided laser can be used to conduct transmyocardial revascularization utilising a percutaneous approach (percutaneous transmyocardial revascularization, or PTMR).
- Transmyocardial revascularization and coronary artery bypass grafting (CABG): Sometimes, coronary artery bypass grafting is done in addition to transmyocardial revascularization (CABG surgery).
Expectations post-surgery:
Transmyocardial laser revascularization will be done at a hospital by a heart surgeon. You will be asleep throughout. While your heart is still beating, your surgeon can do transmyocardial laser revascularization.
The side of your chest will be cut by the doctor, who will then put a laser through it. Your surgeon uses a laser to cut 20 to 40 channels in the wall of the left ventricle, the bottom chamber of your heart. In a short amount of time, a blood clot swiftly seals the channels' outside ends. As a result, the pathways that deliver oxygen-rich blood from within the heart to the heart muscle are blocked. It takes two hours to complete the process.
The risk of complications following cardiac surgery includes heart attacks.
Recovery post-surgery:
Three to ten days are common for hospital stays following transmyocardial laser revascularization. Whether you undergo the operation alone or in conjunction with bypass surgery will be the deciding factor in this. You'll spend a portion of your stay in an intensive care unit.
To aid with your recovery after discharge, your doctor could suggest that you enroll in a cardiac rehabilitation program. After transmyocardial laser revascularization, your doctor may probably restrict your activities for a few weeks. A full recovery could take three months or longer. It is crucial to adhere to heart-healthy rules for life.
Most patients can resume activities that previously gave them chest discomfort. In fact, after a year, 80 to 90 percent of patients still report feeling better than they did before surgery.
Conclusion:
The TMLR method is no longer experimental. Long-term follow-up information is now being gathered after several studies have been completed. A history, a physical examination, and assessments of angina and quality of life are all parts of routine follow-up care. Exercise tolerance testing, thallium scanning, and an array of other exams are routinely carried out. It is still unclear if TMLR significantly affects the mortality rate in this patient population.
Patients gain from the collaboration between medical cardiologists, interventional cardiologists, cardiovascular imaging specialists, radiologists, and anesthesiologists in addition to the expertise of cardiac surgeons. To deliver exceptional results for the patients, they collaborate with nurses, physician assistants, physical therapists, nutritionists, and social workers.