You'll Never Believe How Uro-oncology Can Save Lives: Understanding Its Role in Treating Urological Cancers!
Urological malignancies, such as those of the bladder, kidney, prostate, and testicles, are among the most prevalent cancers worldwide. According to American Cancer Society projections, there will be 609,820 cancer deaths and 1,958,310 new cancer cases in the United States in 2023. However, developments in Uro-oncology have transformed how prostate cancer is treated, leading to better patient outcomes and survival rates. You must thoroughly understand Uro-oncology to comprehend its best consequences and accomplishments.
What is Uro-oncology?
Diagnosing and treating malignancies of the testicles, penis, prostate gland cancer, bladder, and kidneys that affect the urinary system and male reproductive organs are the primary goals of the specialist medical discipline known as Uro-oncology. Doctors who specialize in the treatment of urologic cancers are known as Uro-oncologists. To provide complete care for patients with prostate cancer, they collaborate closely with urologists, radiation oncologists, medical oncologists, and pathologists. Uro-oncology seeks to treat urologic tumors with individualized care that is efficient and successful in terms of patient quality of life. These include targeted medicines, chemotherapy, radiation therapy, and surgical procedures. To create better treatments and increase our knowledge of urologic malignancies, Uro-oncologists also carry out research.
Recent trends of how Uro-oncology is contributing to Urological Cancers
- Personalized Medicine: Using genetic and molecular data to customize treatment for each patient, personalized medicine is a new development in Neuro-oncology. Uro-oncologists can pinpoint specific abnormalities or gene expression patterns that may be causing the formation of prostate cancer by analyzing a patient's genetic makeup. This enables the development of targeted medicines, which may be more efficient and have fewer side effects than conventional chemotherapy or radiation.
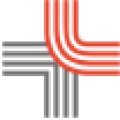
- Minimum Invasive Surgery: Adopting minimally invasive surgical methods, such as laparoscopic and robotic-assisted prostate surgery, is another trend in Uro-oncology. These procedures eliminate malignant tissue while protecting good tissue by making tiny incisions. Compared to open surgery, this causes less discomfort, quicker recovery, and fewer complications.
- Immunotherapy: In prostate cancer treatment, immunotherapy—a more recent form of cancer therapy in Uro-oncology—has produced encouraging outcomes in treating Urological cancers. It involves attacking cancer cells with the body's immune system. Immunotherapy is a treatment option offered by Uro-oncologists for prostate, kidney, and bladder cancers. This method can be helpful even in advanced stages of cancer and has fewer adverse effects than conventional chemotherapy.
- Individualized Therapy Programs: In Uro-oncology, individualized treatment approaches are becoming increasingly prevalent. Uro-oncologists collaborate with other medical specialists to create customized treatment programs to meet each patient's needs. Depending on the type, stage, and severity of cancer, this may require a mix of surgery, chemotherapy, radiation therapy, and other prostate cancer treatments. Personalized treatment regimens can enhance results and lower the chance of unwanted effects.
- Telemedicine: Through video conferencing, telemedicine is a developing trend in Uro-oncology, enabling patients to get care remotely. This is crucial for prostate cancer patients who might be unable to travel to a hospital for treatment. Telemedicine can be utilized for consultations, follow-up appointments, and patient monitoring for problems or adverse effects.
- Biomarkers: Another development in Uro-oncology is biomarkers, a biological indicator that can be used to identify urological malignancies and track their development. To detect symptoms of prostate cancer early and track treatment response, Uro-oncologists use biomarkers like PSA (prostate-specific antigen) and BTA (bladder tumour antigen) for bladder cancer.
- Genetic counselling: The Uro-oncology has also developed genetic counselling for individuals with a family history of urological malignancies. Uro-oncologists collaborate with genetic counsellors to educate patients about their risk of developing prostate cancer and guide them in selecting genetic tests and prevention strategies.
- Comprehensive Care: Often, treating urological malignancies requires a multidisciplinary approach. Medical oncologists, radiation oncologists, pathologists, and radiologists collaborate closely with urologists to offer patients complete and coordinated care.
- Therapeutic Trials: A crucial part of Uro-oncology research is clinical trials. Clinical trials to assess novel medicines and treatments for urological cancers are developed and carried out by Uro-oncologists. Clinical trials provide urological prostate cancer patients with access to cutting-edge therapies that would not be found elsewhere.
- Caring for Survivors: A crucial component of Uro-oncology is survivorship care, which concentrates on the patient's physical and psychological requirements following prostate cancer treatment. To give patients continuous treatment and support, including monitoring for cancer recurrence, managing side effects, and addressing psychological and social problems, Uro-oncologists collaborate with survivorship care teams.
- Cryo-EM: Another technological trend that Uro-oncology use is Cryo-EM, it creates high-resolution pictures of molecules' behaviour to guide Uro-oncology treatment in cancer for better understanding of how cancer cells develop, endure, and interact with treatments and other cells. Cryo-EM has high resolutions and can take pictures of molecules ten thousand the breadth of a human hair. By using 3-D images of molecules that enable scientists to investigate the behaviour of cancer by analysing hundreds of thousands of cryo-EM pictures for quality.
- Infinium Assay: This process in Uro-oncology provides essential insights into how genetic variations relate to cancer. Infinium Assay is a process and set of tools that analyse millions of single nucleotide polymorphisms, or SNPs, the most common type of genetic variation. SNPs can be used to identify cancer-causing genes and shed light on the formation, progression, and risk of the prostate cancer.
Conclusion
It's crucial to contact a healthcare physician as soon as you can if you or someone you know is exhibiting signs of prostate gland cancer. The Department of Urology offers cutting-edge urological cancer testing and treatment services. You may also speak with the skilled Uro-oncologist, Dr. ABCD, who can create individualized treatment plans based on each patient's requirements. Remember that treating urological tumors successfully depends on early detection of the condition, so make an appointment right away.