All you need to know about Bone Marrow Transplant
What is bone marrow?
Bone marrow is the delicate, soft, and spongy tissue that is found inside the central portion of bones and acts as a development and storage space for the body’s blood cells. Bone marrow produces the white blood cells that are responsible for fighting infection, red blood cells that carry oxygen and platelets that stop bleeding in case of injury. There are certain illnesses and treatments that may cause damage to the bone marrow, leading to the need for a bone marrow transplant procedure.
What is bone marrow transplant?
A bone marrow transplant is a medical management and usually does not require any type of surgical management. This stem cell transfusion of healthy bone marrow cells to replace the abnormal cells in a patient has been performed successfully since 1968 to treat various types of diseases and cancers such as leukemias, lymphomas, immune deficiency disorders, and so on.The stem cells which are responsible for production and development of blood cells, found in the bone marrow of donor or patient are taken, filtered, and given back to the patient or same person affter conditionning. Bone marrow transplantation is an intensive procedure with a lengthy recovery time, and bone marrow transplant cost is also a consideration in some cases.
What diseases are treatable by bone marrow transplant?
A bone marrow transplant can be effective or only treatment against certain diseases and multiple types of cance. The advancement of science in last decade leads to the discovery of more diseases that may be benefitted by a bone marrow transplant. Meanwhile, some of the following diseases are being treated using this therapy:
- Acute myeloid Leukemia, Acute Lymphoblastic leukemia
- Various types of Lymphoma
- Multiple Myeloma
- Aplastic Anemia
- Some Solid Cancers
- Immune Deficiency Disorder
- Sickle Cell Anemia and Thalassemia
- Inherited Metabolic Disorder
What are the uses of bone marrow transplant?
Bone marrow transplant procedure has several benefits and uses, accompanied by risks that need to be weighed by a specialist doctor. The following are various principles involved in bone marrow transplant procedure:
- Donor stem cells replaced the diseased and abnormal bone marrow cells with healthy and functional bone marrow stem cells
- The stem cells regenerate a newer immune system, making it capable of fighting leukemia cells that has not been destroyed by radiation or chemotherapy
- Bone marrow transplant helps with a process called rescue, which replaces and restores normal bone marrow function after severe and high dose chemotherapy and radiation have been administered to treat various cancer.
- Bone marrow transplant can effectively replaced genetically damaged bone marrow with healthy bone marrow
Types of bone marrow transplant
Bone marrow transplant can be performed through a number of methods and is dependent on the nature of the donor. The different types of bone marrow transplant procedure are as follows:
- Autologous bone marrow transplant: This process involves when the patient ownself act as bone marrow donor. Stem cells are procured from the patient by collecting stem cells from periphery using apheresis. These stem cells are then either stored or frozen, and given back to the patient after giving transplant conditioning including high dose chemotherapy.
- Allogeneic bone marrow transplant: This transplant type is used when the patient and donor share the same genetic type. Stem cells are procured from a genetically matched donor, relative like a brother or sister or unrelated when are strangers or not related to each other.
- Umbilical cord blood transplant: This transplant involves a process wherein immature stem cells are collected from an umbilical cord immediately after delivery, tested, typed and frozen until they are needed. Such stem cells procured from the umbilical cord are not required to be a very close genetic match.
Bone marrow transplant procedure
The bone marrow transplant procedure is similar to a blood transfusion and is performed over a period of several days. The stem cells are collected preferably in advance of the treatment day, whether a donor is used or the patient’s own cells. Patient is first be given high dose chemotherapy and/or radiotherapy called conditioning as a part of transplant process to knocked out the diseased or damaged patients bone marrow, therefore making space for new stem cells. These procedure weakens the immune system of the patient, and thus requires to be hospitalised in an isolated space with special facilities including HEPA filters to reduce the risk of life threatening infections.
The donor stem cells are then transplanted through infusion by using a central venous catheter that allows the cells to enter the bloodstream and reach the bone marrow. Once the transplant has been performed successfully, great care has to be taken to prevent infections and complications.
Risks and complications
A bone marrow transplant is a major medical procedure that may lead to certain complications during or after the procedure. Overall bone marrow transplant procedure requires the to spend several weeks in the hospital as they are susceptible to life threatening infections and requires close monitoring. Various factors influence the probability of developing complications, like the age of the patient, disease status, overall health status, the type of the transplant. Each individual reacts differently to the transplant process and may experience different symptoms and complications.
Collection of stem cells requires preparation including injections to mobilise stem cells from bone marrow to peripheral blood. During this time patient may experience pain, chills, fever, or flu-like symptoms. Collection of stem cells are usually done using central venous catheter that includes risk of bleeding and pain. The complications related to conditioning are same as usual of high dose chemotherapy and includes vomiting, nausea, loose motion, mucositis, risk of infection and bleeding, or hair loss. The stem cell infusion includes risk of infusion reaction, vomiting, chills or rigors, hives or chest pain. Physical conditions like nausea, vomiting, diarrhea, mouth sores, weakness or mental conditions like emotional distress and temporary mental confusion may also manifest. Bone marrow transplant process involves life threatening risk as well incluuding sepsis, bleeding in vitals organs and may rrequire ICU care and risk of death. Some of the complications that are likely to happen either alone or in combination are:
- Infections: Severe bone marrow suppression may lead to various types of infections. These infections can prevent or delay the engraftment process and also cause permanent damage to the organ. For an immunosuppressed patient, bacterial, viral or fungal infection can be life-threatening.
- Low platelets and red blood cells: These conditions are a result of depleted or non-functioning of the bone marrow. They are managed with blood product transfusion and usually are manageable. Although they can be life threatening with rsik of cardiac failure or bleeding in vital organs including lungs, brain or GI tract.
- Pain: Mouth sores and gastrointestinal (GI) irritation due to high doses of chemotherapy and radiation can cause pain and discomfort.
- Respiratory distress: The lungs and pulmonary system of the body can be seriously affected for reasons like infection, inflammation, and bleeding and may potentially be life threatening.
- Multi Organ damage: The transplantation process may cause temporary or permanent damage to vital organs like the liver, kidney and heart. Infection, fluid graft-versus-host disease, high doses of chemotherapy and radiation may be the cause behind such organ damage.
- Graft failure: is a serious complication that may be life thrreatening. It results when the patient immune system or infection causes loss of donor stem cells and causes failure of engraftment.
- Graft-versus-host disease: This is a serious complication of a bone marrow transplant and can be life-threatening in certain cases. This happens when the donor's transplanted immune system reacts against the patient’s system and attacks the patient’s body and all its organs. The most common sites for GVHD are the GI tract, liver, skin, and lungs.
A bone marrow transplant is a major medical procedure where the prognosis and long term survival is dependent on various factors.
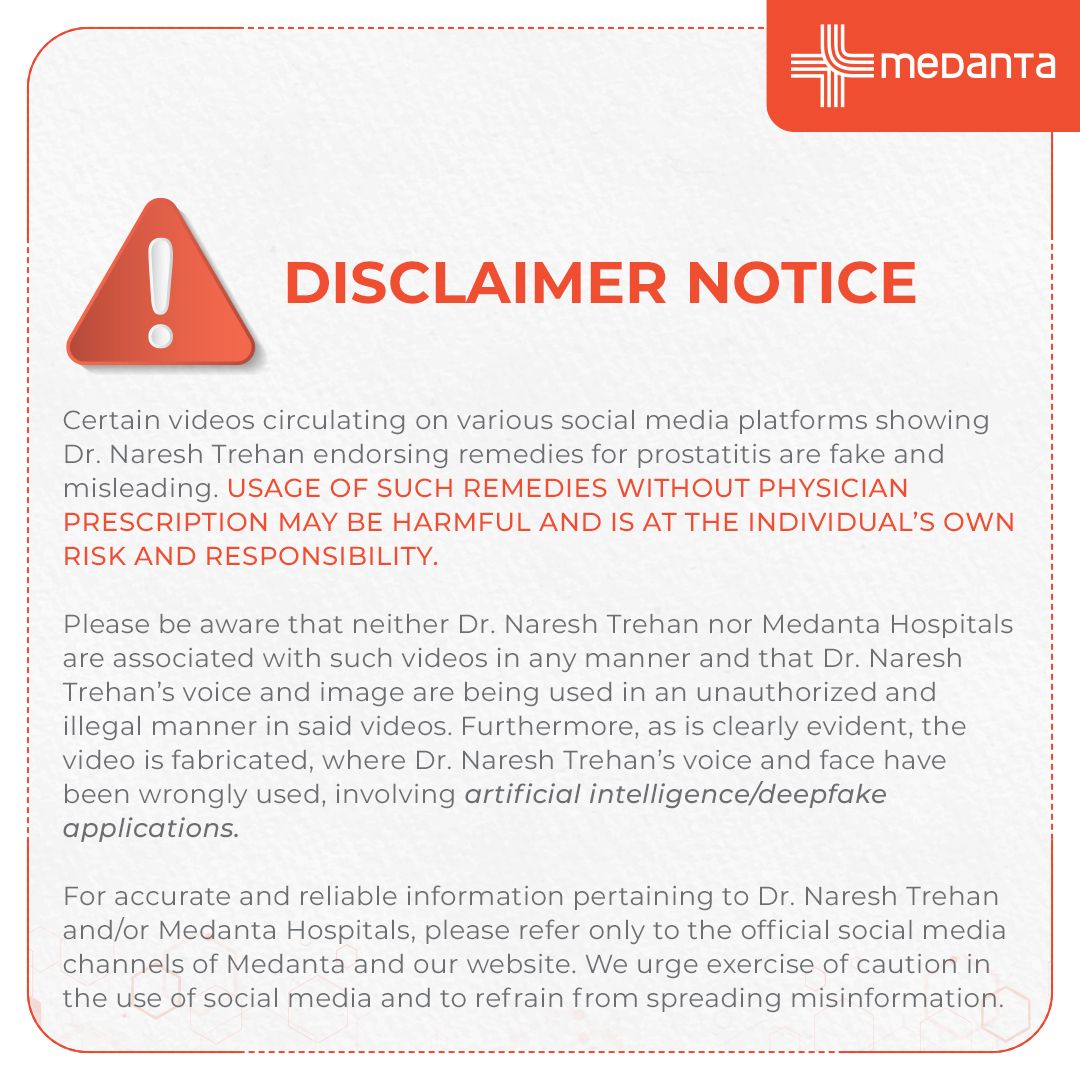
At Medanta Medcity, there is a team of specialists that help with preparation and provide guidance about bone marrow transplant, its need and type of transplant for particular patient and disease. At Medanta’s cancer treatment centre patients have the benefit of state-of-the-art infrastructure, highly specialized team comprising of top haemato- oncologists, with expertise in managing all types of bone marrow transplant and its complications. We have extensive experience in standard and novel therapies to ensure that the care plan offers the best possible outcomes for our patients. Here we focus on the distinct needs of our patients to provide best transplant treatment with maximal comfort, and help to find a donor, if needed to our patients at reasonable cost.