Overcoming Urinary Incontinence Challenges in Elderly Females
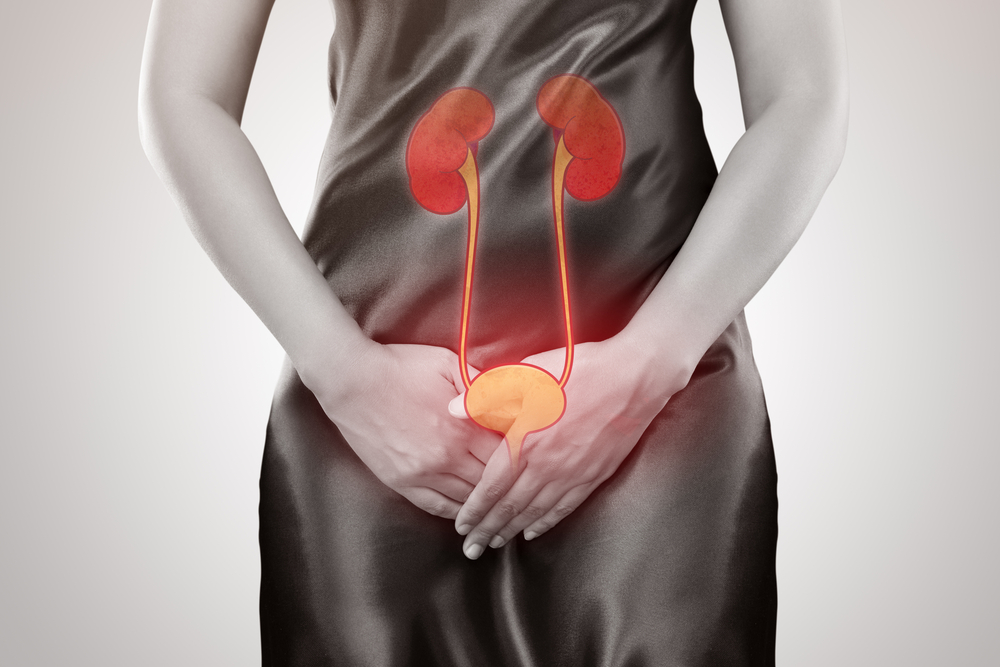
Ageing gracefully is a beautiful journey, but it often comes with its share of challenges. One such challenge that many elderly women face is urinary incontinence. This condition, characterised by the involuntary leakage of urine, can significantly impact your quality of life. In this blog, we’ll talk about urinary incontinence in elderly females and discuss effective strategies to overcome these challenges.
What Is Urinary Incontinence?
Urinary incontinence is when urine is involuntarily lost, ranging from occasional leaks to a complete lack of control. It affects various age groups but is more prevalent in older adults, particularly women.
Types of Urinary Incontinence
- Stress Incontinence: This occurs during physical activities like sneezing, laughing, or exercising, applying pressure to the bladder and leakage occurs due to opening of urethra (bladder pipe) against this rise in bladder pressure as urethral supports required to maintain it in closed state are weakened..
- Urge Incontinence: Involves a sudden, intense need to urinate, often followed by unintentional leakage, caused by unwanted bladder muscle contractions.
- Overflow Incontinence: Results from incomplete bladder emptying, leading to frequent dribbling on bladder overfilling, possibly due to weak bladder muscles.
- Functional incontinence: This type occurs when physical or mental impairments prevent a person from reaching the toilet in time. This may be common in the elderly or individuals with mobility issues or cognitive disorders.
- Mixed incontinence: This is a combination of different types of incontinence, usually a mix of stress and urge incontinence.
Seeking Professional Help
Addressing urinary incontinence begins with seeking professional guidance. Healthcare experts play a vital role in evaluating the seriousness of a condition and creating fitting treatment strategies. Many co-morbid conditions of elderly like cognitive issues, restriction of mobility, compromised cardiac function and medical conditions like uncontrolled diabetes and hypertension might pose as a challenge and should be taken into consideration while deciding appropriate management.
Seeking guidance from a healthcare professional is crucial for multiple reasons. They can exclude hidden medical issues, evaluate the nature and intensity of incontinence, and suggest appropriate interventions. Neglecting symptoms or trying self-diagnosis might result in delayed or ineffectual treatment on one hand and irreversible consequences / complications on another hand. For example, the eldery may fall while rushing to the washroom leading to even fractures.
Medical evaluations might involve an intricate medical background, physical checks, and diagnostic examinations like urine analysis, ultrasound, or urodynamic studies. These assessments aid in pinpointing the underlying cause of incontinence and steer the formulation of tailored treatment plans.
Customised Treatment Plans
Following an evaluation, healthcare experts might suggest personalised treatment approaches.
- Medications: For medications, anticholinergics or beta-3 agonists may be prescribed to stop unwanted bladder contractions and minimise leakage, depending on the incontinence type. It’s very important for elderly to decide the most suitable medication with least side effects, especially when they are already on multiple medications.
- Physical Therapy: This may involve crucial pelvic floor exercises (Kegel exercises) to enhance the strength of pelvic floor muscles, leading to improved urethral closure both at the time of high intra-abdominal pressure like sneezing, coughing, jumping or heavy weight lifting as well as during unwanted bladder contractions.
- Surgical Options: In some cases, surgical interventions like sling procedures, bladder neck suspension or bladder injections of botulinum toxin may be considered to provide additional support to the bladder and urethra.
Lifestyle Modifications
In addition to professional interventions, certain lifestyle modifications can significantly contribute to managing and overcoming urinary incontinence.
Dietary Changes for Bladder Health
- Drinking Habits: Maintaining adequate fluid intake is essential for overall health, but managing when and what you drink can help minimise incontinence episodes. Avoiding excessive caffeine and alcohol intake, especially in the evening, can reduce bladder irritation and urgency.
- Bladder-Friendly Foods: Certain foods, like spicy foods, citrus fruits, and artificial sweeteners, can irritate the bladder. Identifying and minimising the consumption of such foods can contribute to symptom relief. Consuming high fibre diet and avoiding constipation also help.
Pelvic Floor Exercises and Their Significance
Frequent pelvic floor workouts significantly help control incontinence. Strengthening these muscles supports the bladder and urethra, enhancing urinary function control, as explained earlier. Recognizing and activating these muscles is a vital part of the process. Supervision by a health care worker/ clinician will help you in doing so, in a right way.
Maintaining a Healthy Weight
Extra weight can worsen stress incontinence by stressing the pelvic floor muscles. Embracing a nutritious diet and exercising regularly can assist in managing weight and enhancing overall health.
Hydration Habits and Their Impact
While staying hydrated is crucial, strategically managing fluid intake in distributed form during daytime and restricting it especially before bedtime to reduce the frequency of night time bathroom visits, may be helpful. However, it's important not to restrict fluids excessively, as dehydration can lead to concentrated dark urine. This might worsen bladder irritation and incontinence.
Assistive Devices and Products
In addition to lifestyle modifications, various assistive devices and products are available to help manage urinary incontinence with comfort and dignity.
- Absorbent Pads and Underwear: Absorbent pads and underwear provide discreet and effective protection against leaks. They come in various sizes and absorbency levels to meet individual needs.
- Catheters: Catheters may be recommended for individuals with specific types of incontinence or bladder dysfunction. Intermittent catheterization can help empty the bladder completely and reduce the risk of leakage/ overflow .
- Bedding Protection: Waterproof bedding protection is essential for preventing damage to mattresses and ensuring a comfortable and hygienic sleep environment.
How to Choose the Right Products?
Selecting the right incontinence products involves considering factors such as absorbency, fit, comfort, and lifestyle. Trial and error may be necessary to find the most suitable products, and consulting healthcare professionals can provide valuable guidance.
Wearing incontinence products discreetly is a priority for many individuals. Choosing products with odour control features, wearing loose-fitting clothing, and incorporating regular changes are strategies to enhance comfort and maintain confidence.
Emotional and Psychological Support
Beyond the physical challenges, urinary incontinence can have a significant impact on emotional well-being. Addressing the associated stigma and seeking emotional support are crucial aspects of overcoming incontinence challenges.
Incontinence is a common condition, yet stigma and embarrassment often surround it. Normalising discussions about incontinence and promoting awareness can contribute to reducing the stigma associated with this health concern.
Open communication with healthcare providers, family members, and friends is essential. Discussing concerns, sharing experiences, and seeking understanding create a supportive environment that positively influences mental and emotional well-being.
Joining support groups or seeking counselling can provide valuable emotional support and coping strategies. Connecting with others who have experienced similar challenges can be empowering and reassuring.
Conclusion
Overcoming urinary incontinence challenges in elderly females involves a multifaceted approach that addresses both physical and emotional aspects. Seeking professional help, implementing lifestyle modifications, utilising assistive devices, fostering emotional support, and staying informed about advancements in the field are key components of a comprehensive strategy.