V-tach: Things You Should Know About Ventricular Tachycardia Treatment
Introduction
It's common to occasionally feel as though your heart is racing too quickly. You can be feeling anxious or you might have just finished a lengthy run. However, ventricular tachycardia, often known as "VT" or "V-tach," a medical condition with an underlying cause, can occasionally be indicated by a rapid heartbeat.
What is ventricular tachycardia?
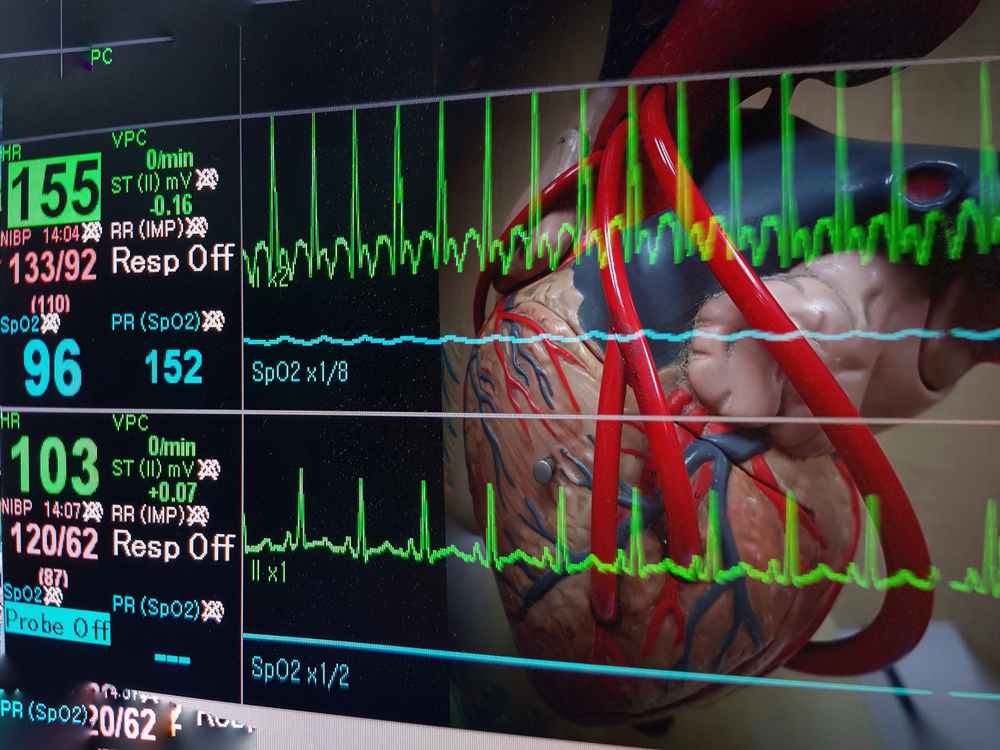
When your heart rate exceeds 120 beats per minute without beginning in the regular electrical pathway, it is said to have ventricular tachycardia.
60 to 100 beats per minute constitute a normal resting heart rate.
When you experience ventricular tachycardia, your heart beats so quickly that:
- Your blood pressure
- Your heart cannot supply your entire body with enough oxygen.
- You begin to have symptoms.
Tachycardia causes
Incorrect heart signalling sets off a rapid heartbeat in the lower heart chambers, resulting in ventricular tachycardia (ventricles). The ventricles cannot fill and contract fully to provide the body with blood because of the rapid heartbeat.
Ventricular tachycardia can result from issues with heart signals that are brought on by a variety of factors. These consist of:
- Cardiovascular disease.
- A heart attack.
- Bigger heart (cardiomyopathy)
- Heart valve dysfunction
- Heart operation
- Certain inherited conditions
- Previous heart attack (myocardial infarction) or heart surgery that made scar tissue on your heart
- Electrical disorders often generate, involving various tissue of heart which is the common cause of sudden cardiac death in young age.
Other non-heart-related causes of ventricular tachycardia include:
- Medications
- Recreational drugs
- Exercise
- Elevated electrolyte imbalance (the minerals that control heart rhythm)
- Alcohol or caffeine in excess
- Extreme stress
There are times when the cause is not known.
Tachycardia symptoms
Blood may not reach the rest of the body adequately if the heart beats too quickly. So the tissues and organs might not receive adequate oxygen. A lack of oxygen causes the signs and symptoms that appear during a ventricular tachycardia episode, which may include:
- Chest pain
- Difficulty breathing
- Palpitations/rapid pulse
- Dizziness
- Lightheadedness, or passing out.
The duration of ventricular tachycardia can range from less than 30 seconds for non-sustained V-tach to more than 30 seconds for sustained V-tach or VT. Short episodes can not result in any symptoms. However, persistent VT might result in major issues, including as
- Fainting
- Loss of consciousness
- Sudden death (Cardiac arrest) which can be revered within few minutes.
Risk Factors
- A history of cardiovascular disease
- Have a family history of problems with cardiac rhythm
- A coronary artery condition
- Have myocarditis
- Experience heart failure
- A heart that is enlarged (cardiomyopathy)
- Have a heart valve condition
- Experienced a myocardial infarction or had heart surgery
- Have serious electrolyte deviations
- Utilize stimulants like methamphetamine or cocaine
Diagnosis
- You should discuss your symptoms
- Perform a physical examination which should include taking your pulse.
- Gather medical history
- Order tests
You'll also have some heart testing.
Your first one will most likely be an EKG. It captures the electrical activity of your heart.
Additionally, your doctor can recommend electrophysiological testing, which identifies trouble spots in your heart.
Tachycardia treatment
If you don't have symptoms or if episodes last less than 30 seconds, you might not need to take any action. If not, how you are treated will depend on the problem's root cause.
You may need to quit taking a prescription or coffee if that is what is triggering your VT.
- To restore your heart's regular beat, your doctor shocks it with electricity. This is a typical emergency treatment, particularly when VT coexists with dizziness or low blood pressure.
- Therapy for cardiac resynchronization (CRT) - A little pacemaker is inserted by your doctor close to your collarbone. To get the ventricles to cooperate as they should, it sends signals to both of them.
- A cardioverter-defibrillator implant (ICD) - This is a little gadget that is positioned beneath your collarbone. It might be included with CRT. If your heartbeat becomes irregular, an ICD shocks you to restore it. It can prevent VT from becoming a potentially fatal issue.
Medications - Your heart rate can be slowed by medications to keep it in a regular rhythm. The serious adverse effects of some medications will be discussed with you by your doctor before the prescription.
- Radiofrequency catheter ablation (RCA) - Your doctor will locate the beginning of an irregular rhythm and then use an electrical current to burn away tissue there with a catheter.
Complications
Although ventricular tachycardia ablation has a long history of success and safety, problems can occasionally occur. Possible complications include:
- Your heart or blood vessel may get damaged
- Blood clots
- Bleeding
- Infection
- Sudden cardiac death
Prevention
- A heart-healthy diet includes one that is high in fruits, vegetables, and whole grains while being low in saturated and trans fats.
- Heart disease risk is increased by being overweight. Aim for at least 30 minutes of moderate exercise each day as a general objective.
- Make lifestyle adjustments and use medications as directed to control high cholesterol or high blood pressure.
- Evaluation of all sudden cardiac death and proper preventive measures.